Highlights from the 2024 POGO Symposium: Through a Nurse’s Lens
By Denise Mills
This year, the POGO Multidisciplinary Symposium on Childhood Cancer took an exciting road trip to Niagara-on-the-Lake, where Ontario’s pediatric oncology community gathered to connect, collaborate, and learn. POGO partner hospitals were well represented, including the five centres with specialized childhood cancer programs and eight POGO Satellite Clinic locations. Over 60 nurses participated in this impactful event! While we can’t relive the Symposium, here are a few key takeaways from the sessions.
Lee Dupuis: The Power of the Patient's Voice in Symptom Management
Lee Dupuis delivered a powerful closing presentation on the critical role of the patient’s voice in improving symptom management. She explained how we define the "patient's voice," how to elicit it from pediatric patients, and why it’s essential to listen and respond effectively to improve care. Lee shared compelling results from a recent trial conducted in the US and Canada, which randomized symptom screening against usual care.

The findings were clear and will be shared in an upcoming publication. For more insights into symptom assessment tools, explore SSPedi and Spark here: Symptom Assessment Tools.
Lee also emphasized the importance of implementing clinical practice guidelines (CPGs) in our clinical practices, such as the Spark Clinical Care Pathways. For more information on CPGs, visit the POGO Clinical Practice Guidelines.

Nicole Culos-Reed: Exercise and Fatigue Management in Pediatric Oncology
Nicole Culos-Reed's session highlighted POGO’s updated CPG recommending physical activity as an effective intervention for fatigue in children and adolescents with cancer. Nicole explored the benefits of exercise during treatment, such as protecting muscle strength, improving immune function, and managing common side effects. She also discussed the long-term importance of physical activity after treatment, including its impact on cognitive function, cardiac health, bone mineral density, and the risk of metabolic syndromes.
To learn more about her POEM program (Pediatric Oncology Exercise Manual) and the IMPACT intervention for physical activity during treatment, visit POEM & IMPACT.
Agnes Wong: The Art and Science of Compassion
Agnes Wong led an inspiring session that guided us through the components of compassion, emphasizing the importance of mental and emotional training for healthcare providers. Agnes also underscored the need for self-compassion as a prerequisite for effectively caring for others. She challenged us to consider how compassion training should be integrated at a systems level, in institutions, and in professional training programs.

For those interested in further developing their compassionate practices, Agnes shared a valuable resource: the Mindfulness & Compassion Training Program at the Sarana Institute.
We hope you find these highlights inspiring and insightful. Thank you to all who attended and contributed to the success of the 2024 POGO Symposium!
Reflective Practice IS Nursing Practice
By: Arvinder Aulakh, Jessica Brooks
“Let us never consider ourselves finished nurses…we must be learning all of our lives.”
Clearly, Florence Nightingale had early insights into the importance of continual professional growth and development. Reflective practice is foundational within pediatric hematology/oncology nursing, enhancing team collaboration, improving care standards, and supporting nurses’ emotional well-being. This offers multifaceted benefits for nurses, their young patients, and the families they care for.
Pediatric hematology/oncology nursing is a profession that embraces collaboration through reflecting on shared experiences and challenges. Reflective practice allows nurses to contribute to the collective knowledge base by critically evaluating their current practices to drive evidence-based practices. Engaging with nurses with different experiences allows for dialogue that contributes to holistic patient care, team learning, and improved communication.
Patient care outcomes are improved through reflective practice. Personal values and beliefs can indirectly and unknowingly affect patient care. Reflective practice provides insights into nurses’ strengths and challenges contributing to better clinical acumen, empathetic communication, and emotional resiliency. Through this, professional growth and development are achieved, allowing for higher standards of patient care.
It is well understood through literature and lived experience that caring for seriously ill children can lead to burnout and compassion fatigue. Reflective practice empowers nurses by enhancing their self-awareness through professional reflection, facilitating peer support through group discussion, and promoting empathy and compassion by providing a safe and non-judgmental environment. Supporting nurses’ well-being through group self-reflection promotes enhanced job satisfaction.
There are many guidelines and frameworks that can be used when doing a reflective practice. When engaging in reflection, nurses should consider these key aspects:
- Description of experience: Recall the important events and features by giving a clear, non-judgmental and comprehensive account of the experience. Experiences may include describing a challenging patient interaction, a successful teamwork experience, or any other significant event.
- Evaluation: Take a “look back” and think about the importance of that experience. What went well? What were the challenges? How did these moments impact patient care, team dynamics, or your personal feelings about work?
- Analysis: An opportunity to critically think about the experience using theory and research. This could include analyzing communication strategies, ethical dilemmas, or case studies that highlight successes and challenges.
- Future action: The experience is summarized to help gain personal insights and determine any next steps. What will you continue to do? What will you change? Setting specific and measurable goals can guide your growth.
Consider incorporating reflective practice into staff meetings, evaluations, and group discussions. Through this, professional development is enhanced because reflective practice IS nursing practice!

About the Authors
Arvinder Aulakh and Jessica Brooks are POGO Interlink Nurses working at SickKids. Learn more about the POGO Interlink Nursing Program.
Spotlight on Tanya Hobson: A Dedicated Advocate for Pediatric Oncology Families in Northern Ontario
Introducing Tanya
For Tanya Hobson, a POGO nurse based at Health Sciences North in Sudbury, caring for young patients with cancer goes far beyond clinical responsibilities. As both a pediatric oncology Satellite Clinic nurse and AfterCare Clinic case manager, Tanya provides essential support for families navigating the challenges of childhood cancer treatment and survivorship in Northern Ontario.
Behind the Care: Tanya’s Daily Impact
In her dual role, Tanya fills her days with clinical duties like, chemotherapy administration and assessments, as well as emotional support that carries into AfterCare. "During treatment, our focus is on helping children manage side effects and supporting families through the process," she says. Post-treatment, her work shifts to help survivors address the long-term effects of cancer treatment, with a special emphasis on maintaining health and well-being for years to come. Reflecting on her work, Tanya shares, “We make a real difference to these families—our work is so valued."

A Unique Path to Pediatric Oncology
Tanya’s path to this role reflects her passion and deep commitment. Initially pursuing medical school, she shifted to nursing to seek a more hands-on, patient-focused career. She gained valuable experience in the Neonatal Intensive Care Unit (NICU) and Intensive Care Unit (ICU) at The Hospital for Sick Children (SickKids) in Toronto for over a decade before moving to Sudbury and discovering her true passion in pediatric oncology. Since then, she has built lasting connections with patients and families in her community, something that she finds deeply rewarding.
Overcoming Challenges in Northern Ontario
Northern Ontario’s vast geography presents unique challenges for healthcare access. Some of Tanya’s patients live up to seven hours away, making trips to the clinic daunting. This distance, coupled with sometimes unpredictable weather and limited access to immediate healthcare resources, requires tailored care that Tanya and her team strive to deliver with dedication.
Addressing Mental Health in Pediatric Oncology
One pressing issue in pediatric oncology, Tanya notes, is the growing need for mental health support. As childhood cancer survival rates improve, families and survivors grapple with the psychological impact of a cancer journey, often extending beyond the treatment phase. Tanya believes integrating mental health support into standard of care is crucial, starting at diagnosis and continuing through survivorship.
Proud Achievements and a Lasting Impact
Reflecting on recent meaningful experiences, Tanya is proud of her recent Canadian Nurses Association (CNA) Certification in Oncology and completion of the Association of Pediatric Hematology/Oncology Nurses (APHON) Chemotherapy/Biotherapy Provider Course. Both credentials affirm her commitment to best practices and a high standard of care for her patients. But her greatest achievement, she shares, came when a former patient recently told her he was pursuing nursing because of the care he received from her. “It was lovely to hear the impact we make,” Tanya says, smiling.
Closing Reflections
In her 10 years in Sudbury, Tanya remains inspired by the resilience of her patients and families. Each day, she brings a compassionate approach to a field she feels called to, embodying POGO’s mission to ensure children with cancer and their families receive the best possible support—no matter where they live.
Improving the Experience: Innovating the Standard Blinatumomab Medical Backpack at SickKids
By: Alia Petropoulosand Lisa Honeyford
Blinatumomab is an immunotherapy primarily used to treat certain types of blood cancers. Its administration necessitates a continuous 28-day infusion delivered on an outpatient basis that families typically can manage at home. Although a standard medical-grade bag is provided to families to hold the device, our clinical team at SickKids identified several design flaws, including poor fit and function for children, along with a distinctly “medical” appearance that can be stigmatizing.
To address these challenges, a grant proposal was submitted to the Garron Family Cancer Centre (GFCC) to improve the experience for families caring for children receiving blinatumomab. Our goal was to understand the challenges families faced going home with a 28-day blinatumomab infusion. We knew that the right carrying bag design could make a significant difference in the daily lives of these patients and maximize the activities they are able to participate in while receiving the medication
Once the project was successfully funded, a dedicated team was assembled, comprising of nurses, an oncologist, a child life specialist, and an industrial designer. Our approach included comprehensive desktop research, product testing, and personal interviews with families to understand their experiences with the current medical bag. The insights gathered after interviewing patients, families, and healthcare providers, led to the creation of a list of criteria for the ideal medical bag. The team then collaborated with an industrial designer to develop a blueprint for a prototype and secured a vendor to produce it for testing.

The new prototype bag was created as a backpack and tested with 10 pediatric patients receiving blinatumomab. Half of the participants began with the standard bag while the other half started with the prototype backpack. The team gathered feedback from frontline nurses and families who completed surveys assessing comfort, function, acceptability, and preference. Remarkably, 9 out of 10 participants preferred the prototype backpack, citing improved fit, comfort, and functionality.
“It really helped my child feel more independent during daily activities,” shared one parent, highlighting the emotional benefits of a well-designed product.
This valuable input guided the industrial designer in creating a second-generation prototype, enhancing the fit, security, and accessibility of the medication and pump, as well as improving how families could set up and wear the bag.
Looking ahead, the project team* is working to secure funding and create a process that will allow the backpack to be accessible to any Canadian child receiving blinatumomab. Canadian sites will be contacted when this step is complete, and backpacks are available for distribution. Future efforts will focus on expanding the availability of the backpack internationally.
[Watch the video The Blina Backpack: Changing how we deliver paediatric immunotherapy treatments]


*Project Team includes Alia Petropoulos, Chantal Campbell, Registered Nurse (RN), Lisa Honeyford and Sue Zupanec, Nurse Practitioner (NP).
About the Authors
Alia Petropoulos and Lisa Honeyford are Interprofessional Education Specialists at SickKids.
Editorial Team Note
Congratulations to the project team who were recently recognized for their innovative intervention, the Blinatumomab Backpack, by way of a SickKids President's Award. The President's Award was introduced in 2011 to recognize staff, teams, students and/or volunteers who demonstrate superior leadership and collaboration resulting in major contributions to the organization.
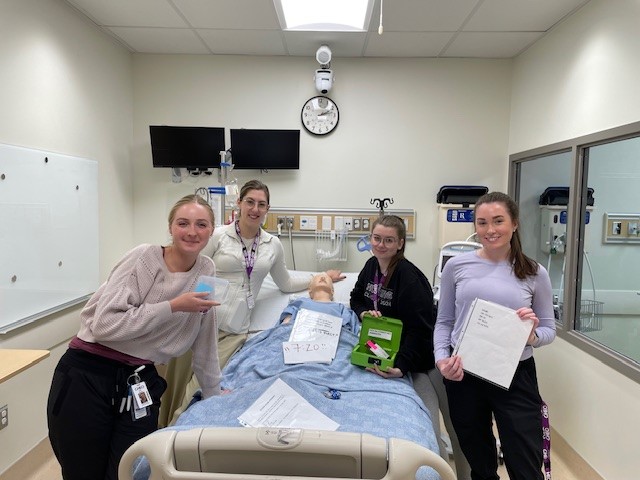
Evaluating Healthcare Simulation Escape Rooms as an Educational Tool in Nursing Continuing Education: A Fellowship Journey
By: Brennah Holley
Fellowship Overview
Brennah Holley, Clinical Nurse Educator at CHEO in Ottawa (and former Co-Chair of the POGO Nursing Committee), recently completed an Advanced Clinical Practice Fellowship (ACPF) through the Registered Nurses Association of Ontario and is now conducting an exciting research project (directly related to her fellowship) to explore the potential of Healthcare Simulation Escape Rooms (HSER) as an innovative educational tool in nursing. With the nursing profession facing pressing challenges such as staffing shortages and varied learning needs, her research aims to assess whether HSERs can enhance knowledge acquisition among nursing staff.
“HSERs merge gamification with traditional learning, creating engaging team-based experiences,” Brennah explains. As defined by Anderson et al. (2020), HSERs infuse healthcare themes into interactive escape room settings, offering a fresh platform for education and assessment.
Research Objective and Methodology
At the heart of Brennah’s research is the objective to evaluate HSERs' effectiveness in nursing education. The study, which began in early 2024, will investigate whether engaging in an HSER focused on anaphylaxis leads to better knowledge retention and application compared to traditional lecture formats.
In a randomized controlled trial, nurses at CHEO will be divided into two groups: Group A will receive a lecture, while Group B will experience both the lecture and the HSER. “This approach allows us to gather vital data on the impact of immersive learning,” she notes.
Learning Experience and Skill Development
Brennah’s journey through the fellowship has been rich with learning. She acquired essential skills in research design, ethics submissions, and statistical analysis. Working alongside the Clinical Research Unit (CRU) at CHEO, she navigated the complexities of ethics applications, completing necessary training and developing vital documentation like consent forms.
Addressing knowledge gaps in statistical analysis was a significant focus for Brennah. By collaborating with a co-investigator from CHEO’s CRU, she enhanced her research capacity. “This partnership has been instrumental in refining my project,” she emphasizes.
Brennah also developed her skills in survey design and literature reviews, both critical for creating effective educational tools.
Outcomes and Future Directions
Data collection for her research will extend until early 2025, with plans to draft a manuscript by fall 2025. The implications of Brennah’s research could be profound, providing evidence to support the integration of HSERs into nursing curricula and continuing education programs. “Ultimately, we want to enhance patient care through improved educational strategies,” she states.
Reflections
Reflecting on her ACPF experience, Brennah describes it as transformative, filled with opportunities for professional growth. Presenting at international conferences and collaborating with nurse educators worldwide have enriched her journey. As she begins her master’s in Nursing, she is eager to further explore innovative educational methodologies, with HSERs leading her efforts to improve nursing practice.
In summary, Brennah Holley’s fellowship at CHEO highlights the promise of innovative educational approaches in nursing, paving the way for advancements in continuing education and enhanced patient care.
“We are on the brink of a new era in nursing education,” she concludes, optimistic about the future.
To learn more about Brennah’s fellowship experience or research endeavours, feel free to reach out to her.